Translate this page into:
A rare case of familial malalignment of the great toenails
*Corresponding author: Sanjeev Gupta, Department of Dermatology Venereology Leprosy, Maharishi Markandeshwar Institute of Medical Sciences and Research, MMDU, Mullana, Ambala, Haryana, India. sanjeevguptadr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dabhra A, Rani N, Mahendra A, Gupta S. A rare case of familial malalignment of the great toenails. J Onychol Nail Surg. doi: 10.25259/JONS_33_2024
Abstract
We report a 27-year-old male presenting with malalignment of the great toenail, a nail disorder characterised by lateral deviation of the nail plate. This case presented a familial clustering of the condition and the cyclic nature of nail shedding. Clinical examination revealed significant thickening, increased curvature, discolouration and lateral deviation of both great toenail plates significantly impacting the patient’s quality of life. There were no predisposing factors including any history of trauma, systemic illness or fungal infection. This case underscores the importance of considering familial predisposition in the evaluation and management of malalignment of great toenails, highlighting the need for further research into its genetic underpinnings.
Keywords
Malalignment of great toenail
Lateral deviation of the nail plate
Nail disorder
Nail matricectomy
INTRODUCTION
In general, nail dystrophy refers to altered or disturbed nail growth caused by a variety of conditions that can affect the matrix and/or bed. One of these conditions is congenital or acquired (traumatic and iatrogenic) malalignment of the nails.[1] First identified by Samman[2] in 1978, congenital malalignment of the great toenail was later reported by Baran et al.[3] in 1979, as a condition where the nail plate deviates laterally from the long axis of the distal phalanx. This rare condition often manifests in childhood or infancy; though later onset is rare. The severity of the case determines the treatment options, which range from conservative to surgical management.
CASE REPORT
A 27-year-old male patient visited the Dermatology Outpatient Department with a concerning history regarding the progressive thickening and increased curvature of his right toenail which deviated laterally. The condition appeared at the age of 17, with no prior abnormalities in nail appearance. He reported experiencing a similar issue with the left toenail around the same time, with no associated trauma. Initially, the patient noticed a slight thickening and discolouration of his toenails; however, as time passed, his nails became increasingly difficult to manage, leading to discomfort and challenges in wearing shoes. He described a recurring cycle lasting approximately 3 years, during which his toenails would grow with increased curvature before naturally shedding without any apparent trauma. There was no history of significant trauma or dermatological conditions such as onychomycosis, psoriasis, ichthyosis, or pemphigus. No history or evidence suggested any systemic illness. The patient also had no history of burns or microtrauma affecting the nails. Despite using various over-the-counter treatments, such as topical antifungals and nail softeners, he experienced minimal improvement. His dissatisfaction and embarrassment regarding the appearance of his nails prompted social withdrawal and avoidance of activities, he once enjoyed. Upon further inquiry, it was discovered that the patient’s elder brother had also experienced similar nail changes around the age of 18 years. Furthermore, the patient’s mother had encountered similar nail abnormalities when she was 20 years old. Interestingly, no history of preceding trauma was reported in either case. Upon closer enquiry, it became evident that a majority of the patient’s family members had experienced similar nail abnormalities around the ages of 16–20 years, with no reported incidents of trauma [Figure 1].
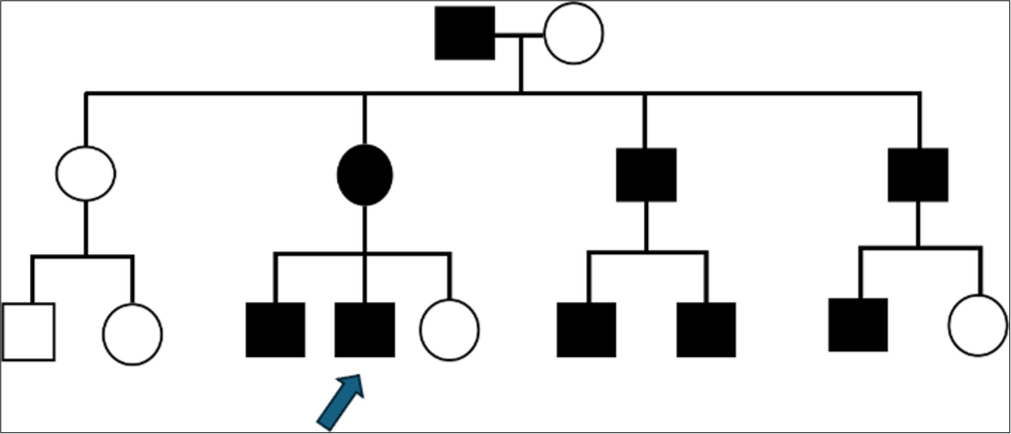
- Pedigree of the family. The index case is indicated by an arrow. Black-filled symbols indicate affected members.
Upon examination, the patient’s toenails displayed significant thickening, increased curvature, discolouration and lateral deviation of both great toenail plates consistent with malalignment of great toenails [Figures 2a and 2b, 3a and 3b]. Nail scrapings and clippings were subjected to potassium hydroxide (KOH) mount for direct microscopic examination, done to rule out onychomycosis, came out to be negative. Nail biopsy was advised; however, the patient refused. The patient was advised to undergo a regimen of regular nail trimming. He was advised total nail avulsion with matricectomy as a part of the treatment plan; however, the patient declined to proceed with it.

- Depicting (a) right and (b) left foot of the patient.

- Showing (a) right and (b) left toenail of the patient. Significant thickening, increased curvature, discolouration of nail plate and malalignment of great toenails.
DISCUSSION
Lateral deviation of the nail plate along the longitudinal axis as a result of a lateral rotation of the nail matrix, is characteristic of congenital malalignment of the great toenails.[2] There have been reports of medial deviation as well.[4] Usually affecting the halluces, but occasionally other toenails, malalignment can be unilateral or bilateral. Repeated microtrauma to the nail matrix causes the nail plate to grow out with transverse ridges. A common sign is nail plate discolouration, which may be exacerbated by infection or haemorrhage.[5] Pseudomonas infection can occur as an opportunistic infection of the nail plate. Inflammation, erythema and pain are often caused due to the malaligned toenail being embedded in the lateral nail fold, leading to acute or chronic paronychia.
Although the precise pathogenesis of congenital malalignment is unknown, a number of theories have been proposed, including environmental factors (such as intrauterine or vascular insult during foetal growth), lateral rotation of the nail matrix and an anomaly in the ligament that connects the matrix to the periosteum of the distal phalanx.[6] A novel theory by Chaniotakis et al.[6] proposed a desynchronised growth between the nail and the distal phalanx of the hallux, which results in a larger nail plate that needs to extend laterally to fit into the underlying bony gap.
Trauma from mechanical means may result in acquired forms of malalignment. A study by Kim et al.[7] concluded that trauma appears to be a significant contributing factor towards acquired great toenail dystrophy. Iatrogenic malalignment has been reported as a consequence of wide lateral nail biopsies or similar excisions, resulting in acquired malalignment of affected nail.[1]
Depending on the severity of the condition, there are many different treatment options. Conservative management options should be explored initially. The patient should be advised to wear comfortable, well-fitting shoes to reduce the chances of repetitive trauma. In severe cases, surgery can be performed, which involves rotating the nail matrix to a proper orientation, allowing the nail plate to grow parallel to the distal phalanx.[1] Surgical correction is advised till the age of 2 years, though this cutoff is flexible.,[1] Another surgical option is total matricectomy. Although the removal of the nail unit completely resolves symptoms, it is not aesthetically pleasant.
CONCLUSION
A familial clustering of the condition, affecting the patient’s family members in their late second decade, without any history of trauma, suggests a genetic predisposition in our case, not commonly reported in the literature. The patient’s progressive nail changes, including thickening, curvature and cyclic shedding over a period of 3 years, add to the rarity of this case, as this cyclic pattern is not a commonly recognised feature. These combined factors make this case particularly notable in the study of malalignment of toenails.
Authors’ contributions
All authors have equally and significantly contributed in making diagnosis, work up of case, literature search, writing and editing of the manuscript
Ethical approval
The Institutional Review Board has waived the ethical approval for this study
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Etiology and treatment of nail malalignment. Dermatol Surg. 1998;24:719-21.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital malalignment of the big toe nail. Clin Exp Dermal. 1979;4:359-60.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital alignment of the big toenail: A new subtype. Arch Dermatol. 1987;123:437.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital malalignment of the great toenails mimicking onychomycosis. J Pediatr. 2005;146:575.
- [CrossRef] [PubMed] [Google Scholar]
- Dizygotic twins with congenital malalignment of great toenails: Reappraisal of the pathogenesis. J Am Acad Dermatol. 2007;57:711-5.
- [CrossRef] [PubMed] [Google Scholar]
- Great toenail dystrophy: A single-center experience and review of the literature. Korean J Fam Med. 2015;36:113-20.
- [CrossRef] [PubMed] [Google Scholar]