Translate this page into:
Habit-tic deformity or median canaliform dystrophy – At a crossroad
*Corresponding author: Diptiranjani Bisoyi, Associate Professor, Department of Dermatology, Sriram Chandra Bhanj Medical College, Cuttack, Odisha, India. diptiranjanibisoyi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bisoyi D, Singh SK, Senapati A, Sahu RR. Habit-tic deformity or median canaliform dystrophy – At a crossroad. J Onychol Nail Surg. 2025;2:57-9. doi: 10.25259/JONS_6_2025
CASE DETAILS
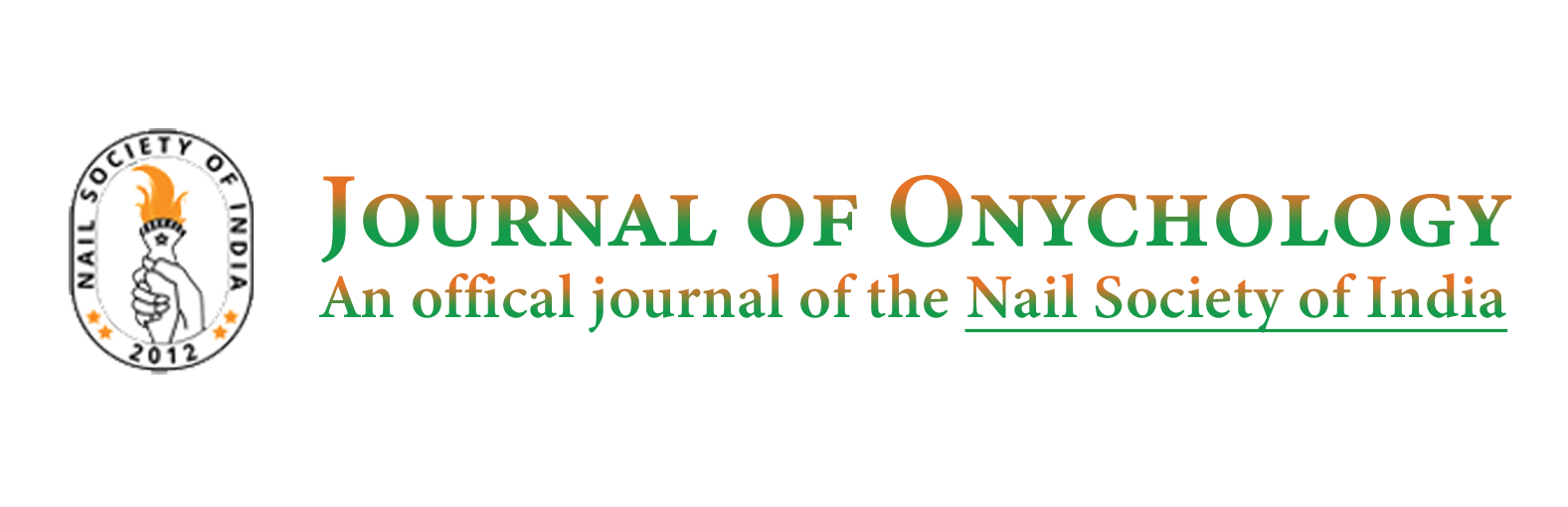
A 9-year-old male child presented to our dermatology department with his mother complaining of dystrophy of the left thumbnail for 6 months. On cross-questioning, parents denied any self-infliction of nails with index fingers. On examination, there were transverse linear grooves and horizontal splits over the nail, an absent cuticle and proximal nail fold disruption on the left thumb [Figure 1].
- 8-year-old male child showing retraction of nail fold (arrow), horizontal splits (upper star) and absent lunula (lower star) of the left thumb nail.
QUESTION
What is your diagnosis?
Median canaliform dystrophy or habit-tic nail disorder/deformity?
DIAGNOSIS
Habit-tic disorder (HTD)
DISCUSSION
A longitudinally depressed groove and transversely parallel ridges that runs from the proximal nail fold to the distal edge of the nail, is characteristic of Habit-tic disorder/deformity. One or both thumbnails are typically involved.[1,2] In severe cases, the cuticle may disappear and the lunula (macrolunula) may grow.[1] Complications include permanent nail dystrophy, infection and frictional melanonychia. It is one of the recurrent nail-related body-focused repetitive behaviours (BFRB); onychophagia and onychotillomania being the others. The World Health Organization’s International Classification of Diseases and Related Health Problems, Eleventh Revision, 2022, included these unidentified BFRBs in its chapter on mental and behavioural disorders. Most individuals with habit-tic deformity are unaware that the cause of their dystrophy is regularly touching the proximal nail fold and its underlying matrix with their neighbouring index finger. The management may involve the use of pharmacological medications and/or non-pharmacologic therapies. To artificially recreate the cuticle and avoid damaging the underlying nail matrix, non-pharmacologic interventions include applying cyanoacrylate adhesive (found in super glue), which is also reasonably priced,[3] or benzethonium chloride (used as an antiseptic) to the nail where the proximal nail fold is present. The physical method of covering the area in paper tape. Benzethonium chloride and paper tape methods are better since cyanoacrylate is known to cause allergic contact dermatitis. Non-pharmacologic treatments, including habit reversal therapy, may also be taken into consideration.[2,4] Tricyclic antidepressants, N-acetylcysteine, antipsychotic drugs and selective serotonin reuptake inhibitors are some of the drugs that have been used. However, the results with various medications differ.[4]
A frequent differential diagnosis for persistent nail deformity is median canaliform dystrophy. We had a similar patient, a 68-year-old male, who presented to us with midline split and ridges radiating outward from the centre, but with minimal nail fold changes, involving bilateral great toe [Figure 2]. Heller’s median canaliform dystrophy is also known as dystrophia unguis mediana canaliformis and nevus striatus unguis. A midline nail plate split with many oblique and proximal outward ridges from the middle of the split nail in a fir-tree pattern, is the condition’s typical appearance.[4,5] The exact aetiology of this uncommon ailment is yet unknown. Table 1 illustrates how these two things differ from one another. According to some authors MCD may result from repetitive trauma, and HTD and MCD are different forms of the same condition.[5] Differentiating them in certain patients can occasionally be challenging.

- A 68-year-old male presented to us with a midline split and outward ridges from the center (arrow) with minimal nail fold changes present over bilateral great toenails.
| HTD | MCD |
|---|---|
| Transverse ridging with central depression and extended, parallel ridges running the full length of the nail. | Transverse ridging with a midline canal resembling an inverted fire tree pattern, with backward angling of | branches.[3,5] |
| Trauma is the main cause. | Trauma to the cuticle and nail matrix may be the cause, but in the majority of cases, the cause is unknown. |
| No familial occurrence and not associated with any drug intake. | Some reports have suggested a familial occurrence and consequence of taking drugs like retinoids.[5] |
| Damaged cuticle, which shows a wider gap between the nail plate and the proximal nail fold. | Damage to cuticle can occasionally result in their enlargement. |
| Hypertrophy of the lunulae (macrolunulae) may be seen.[1] | Thickening of the proximal nail fold, enlargement and redness of the lunula may be seen. |
| Changes in nail folds are more hyperkeratotic.[3] | Although nail fold alterations are possible, the nail fold and surrounding tissue are often normal. |
| Thumb nails are most commonly affected. | Thumbs and great toes are affected. |
| Often asymmetrical. | Mostly symmetrical. |
| Psychodermatoses such as trichotillomania, onychophagia, and OCD may be linked to HTD. | Occasionally, longitudinal grooves and lifting of the nail plate from the nail bed can also be caused by subungual skin tumours, such as glomus and myxoid tumours.[5] |
| Following nail picking, patients with HTD may experience a sense of relaxation. | There is no evidence of such behaviour.[4] |
| In addition to benzethonium chloride and paper tape treatments, treatment may involve a combination of behavioural, psychological, pharmacological and barrier therapies. | Most often, topical Tacrolimus and Tazarotene are recommended. Self-inflicted trauma can be treated in accordance to HTD if that is the cause. |
HTD: Habit-tic deformity, MCD: Median canal dystrophy, OCD: obsessive-compulsive disorder
Authors’ contributions:
All the authors have contributed in writing the manuscript, editing, analysing and curating ideas for the quiz.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Clinical pearl: Benzethonium chloride for habit-tic nail deformity. Cutis. 2019;104:81-2.
- [Google Scholar]
- Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146:1222-3.
- [CrossRef] [PubMed] [Google Scholar]
- Nail tic disorders: Manifestations, pathogenesis and management. Indian J Dermatol Venereol Leprol. 2017;83:19-26.
- [CrossRef] [PubMed] [Google Scholar]
- Median canaliform dystrophy of Heller. Indian Dermatol Online J. 2012;3:224-5.
- [CrossRef] [PubMed] [Google Scholar]