Translate this page into:
Modified dermatology life quality index in patients with nail disorders
*Corresponding author: Dr. Navya Donaparthi MD DNB DVL, Associate Professor, Department of Dermatology, Command Hospital, Airforce, Bengaluru, Karnataka, India. navya.donaparthi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar R, Arora S, Janney MS, Donaparthi N. Modified dermatology life quality index in patients with nail disorders at a tertiary care hospital. J Onychol Nail Surg. doi: 10.25259/JONS_15_2024
Abstract
Background
Skin diseases impact lives physiologically, socially and psychologically compromising quality of life (QoL). Nails are important epidermal appendages and their disorders contribute to a decrease in QoL. Hence, it is imperative to assess their impact.
Objectives
To study the modified DLQI in patients with nail disorders.
Materials & Methods
A single-centre, questionnaire based cross-sectional study was conducted at a tertiary care outpatient department over 18 months. Patients with diagnosed nail disorders in the age group of 18-60 years, of either sex, were included in the study and administered a pre-validated questionnaire (designed based on the Dermatology Life Quality Index (DLQI) questionnaire and validated by a departmental pilot study). Based on the responses marked, the total score was calculated, and patients were categorised into specific band groups, namely, 0-1 = No effect on QoL, 2-5 = small effect, 6-10 = moderate effect, 11-20 very large effect and 21-30 = extremely large effect. Data were analysed using the Statistical Package for the Social Sciences version 22.2 and correlated with the clinicodemographic profile.
Results
A total of 200 patients completed the study. Onychomycosis was the most common presentation (52.5%), followed by acute paronychia (23.5%) and nail psoriasis (18%). Higher modified DLQI scores were found in females with fingernail involvement, students and housewives. The number of nails affected and the duration of nail disorders followed an inverted bell-shaped pattern, with higher modified DLQI scores observed at both the lower and higher extremes. Overall, the impact of nail disorders showed a moderate effect on mean modified DLQI with a mean (range) of 6.9 (6-10).
Conclusion
Nail disorders, having a prolonged disease and treatment course had a moderate effect on the modified DLQI.
Keywords
Quality of life
Dermatology life quality index
Nail disorders
Onychomycosis
INTRODUCTION
Quality of life (QoL), as defined by the World Health Organization, encompasses an individual’s perceptions of their life position, considering personal goals and standards within their cultural context.[1] Clinical practice often prioritizes physical health, yet mental and social well-being, though equally vital, are often overlooked. Dermatological conditions, including nail disorders, can significantly impact an individual’s self-esteem, functionality and social interactions, further underscoring the relevance of QoL assessment in dermatology.[2,3]
Nail disorders, comprising around 10% of dermatologic cases, involve various pathologies affecting the nail unit, with onychomycosis and nail psoriasis being the most prevalent.[4] Nail disorders can also occur in many other dermatological conditions, for example, alopecia areata, atopic eczema, pityriasis rubra pilaris, or it can be seen as a manifestation of many systemic illnesses such as chronic lung disease, chronic renal disease, chronic ischemic heart disease, liver cirrhosis, malnutrition and can also be secondary to drugs.[5,6] Although past research has focused on individual nail conditions, few studies encompass the broad spectrum of nail disorders and their cumulative impact on QoL.[4]
The dermatology life quality index (DLQI) is a simple, validated 10-item questionnaire used to assess the QoL impact of dermatological conditions.[7] The modified DLQI applied here allows for a nuanced understanding of QoL in nail disorders, acknowledging both psychological and functional effects. Given the psychosocial and professional disruptions caused by nail conditions, this study aims to quantify their impact on patients’ QoL and evaluate how it varies based on clinical and demographic factors.
MATERIAL AND METHODS
The study was conducted as a single-centre, questionnaire based cross-sectional study over 18 months, at a tertiary care hospital. Consenting patients of age group 18–60 years, presenting with nail disorders to the dermatology outpatient department were included in the study.
Sample size was estimated with a confidence level of 95%, margin of error of ± 7.5%, and drop out rate of 15%. Convenience sampling was done and the study included outpatient with clinically diagnosed nail disorders, aged 18-60 years of either sex, attending the dermatology outpatient department and willing to participate in the survey. Exclusion criteria encompassed children under 17 years of age and elderly individuals above 60 years.
The clinicodemographic profile of the participants was documented. The questionnaire was designed for this study, on the lines of DLQI [Annexure 1]. Permission was taken from the owners regarding the modification. Participants were instructed to choose the most appropriate response describing the impact of the nail disorder on their QoL in the past 1 week. Based on the response marked, each question was given a score of zero to three, with zero assigned to ‘not at all’,’ no’ or not relevant’; one assigned to ‘a little’; two assigned to ‘a lot’; and three assigned to ‘very much’. The total score was calculated (min 0–max 30), and patients were categorised into specific band groups, namely, 0–1 = no effect on patient’s life, 2–5 = small effect, 6–10 = moderate effect, 11–20 = very large effect and 21–30 = extremely large effect. Data obtained were analysed using the Statistical Package for the Social (SPSS) 22.2 and correlated with the clinicodemographic profile.
RESULTS
A total of 200 patients with nail disorders belonging to the age group 18–60 years were included in the study. The majority of the study subjects belonged to the age group 51–60 years, and there were a greater number of males, 115 (57.5%), as compared to 85 female patients (42.5%). The demographic profile of the patients as per educational qualification and profession was recorded and is depicted in Figures 1 and 2.
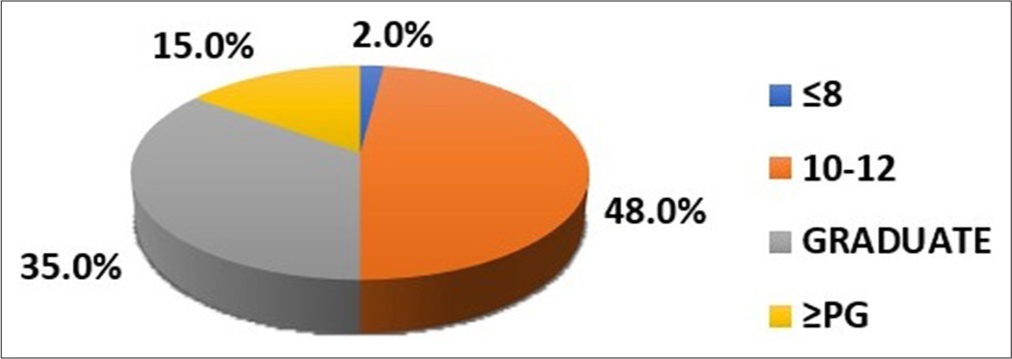
- Distribution of cases as per educational qualification.
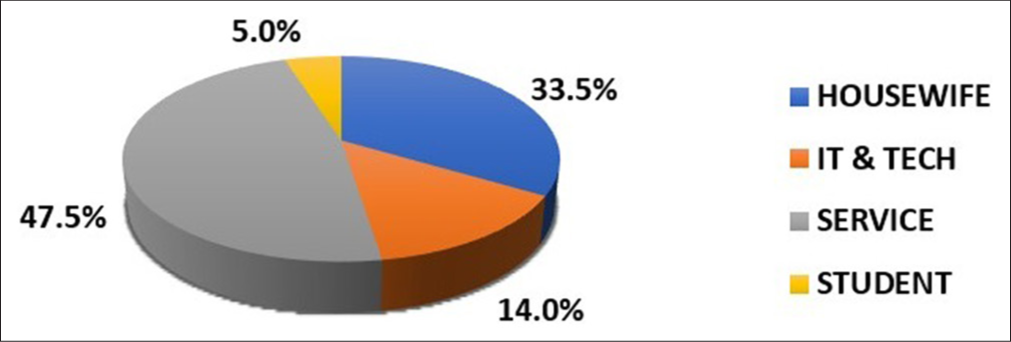
- Distribution of cases as per profession.
A large variation in the duration of nail disorder was found in the patients ranging from 01 month to 120 months with a mean of 21.8 months. Patients had a range of involvement of nails varying from 01 nail to all 20 nails involved, with a mean of 3.1 nails. Onycholysis was the commonest encountered nail change (seen in 67.5% of patients), along with other changes such as nail dystrophy, nail plate thickening, subungual hyperkeratosis and melanonychia. Onychomycosis was the most common diagnosis in the study patients. The distribution of nail disorders is given in Table 1. The patient scored each of the 10 questions of the modified DLQI questionnaire, and the mean score for each question, and the total score for each patient, was calculated. The mean modified DLQI score was 6.9±5.5 against the maximum score of 30 [Table 2]. The highest value of mean response was found for question 2 which assessed the level of embarrassment/self-consciousness due to the nail condition (1.6±1.1) [Table 2]. The highest mean modified DLQI was observed in the age group 21–30 years, which is 9.5±4.0 [Figure 3]. The total score showed statistically significant variation with age group (p<0.001). On comparing the modified DLQI variation between sexes, females were found to have higher scores than males (7.5 and 6.4, respectively). However, the difference was not statistically significant (p=0.18). Statistically significant variation was noted in mean modified DLQI scores as per the duration of illness, number of nails involved, and the profession of the patients, as depicted in Table 3. However, the variation based on the educational qualifications of the patients was not statistically significant (p=0.052).
| Disease | Number of patients | % |
|---|---|---|
| Onychomycosis | 105 | 52.5 |
| Paronychia | 47 | 23.5 |
| Ingrown toenail | 41 | 20.5 |
| Nail psoriasis | 36 | 18 |
| Idiopathic | 4 | 2 |
| Trachyonychia | 4 | 2 |
| Total | 200 | 100 |
| Questionnaire | Min | Max | Mean | SD |
|---|---|---|---|---|
| Q1: How itchy, sore, painful or stinging have your nails been? | 0 | 3 | 1.1 | 1.0 |
| Q2: How embarrassed or self-conscious have you been because of your nails? | 0 | 3 | 1.6 | 1.1 |
| Q3: How much have your nails interfered with you going shopping or looking after your home or garden? | 0 | 3 | 0.9 | 1.0 |
| Q4: How much have your nails influenced the clothes you wear? | 0 | 3 | 0.4 | 0.8 |
| Q5: How much have your nails affected any social or leisure activities? | 0 | 3 | 0.5 | 0.9 |
| Q6: How much have your nails made it difficult for you to do any sport? | 0 | 3 | 0.5 | 0.9 |
| Q7: Have your nails prevented you from working or studying? | 0 | 3 | 1.0 | 1.4 |
| Q8: How much have your nails created problems with your partner or any of your close friends or relatives? | 0 | 3 | 0.5 | 0.8 |
| Q9: How much have your nails caused any sexual difficulties? | 0 | 3 | 0.2 | 0.6 |
| Q10: How much of a problem has the treatment for your nails been? | 0 | 3 | 0.2 | 0.6 |
| Total score | 0 | 30 | 6.9 | 5.5 |
SD: Standard deviation
| Parameters | Total score (mean±SD) | P-value | |
|---|---|---|---|
| Education | ≤8th standard | 3±0 | 0.052 |
| 10–12 standard | 6.1±4.6 | ||
| graduate | 7.1±5.4 | ||
| ≥Postgraduate | 9±7.6 | ||
| Duration (months) | 1–2 | 8.1±7.3 | 0.001* |
| 3–5 | 5.7±4.3 | ||
| 6–12 | 5.4±4.3 | ||
| 12–24 | 8.7±1.3 | ||
| 24–60 | 9.8±4.8 | ||
| >60 | 9.8±9.1 | ||
| Number of nails | 1–5 | 6.7±5.3 | <0.001* |
| 6–10 | 3.1±2.2 | ||
| >10 | 14±5.3 | ||
| Profession | Housewife | 7.2±4.6 | 0.001* |
| Information Technology/Technology | 4.6±3.1 | ||
| service industry | 6.5±6.6 | ||
| Student | 11.7±0.5 | ||
| Total | 6.9±5.6 | ||
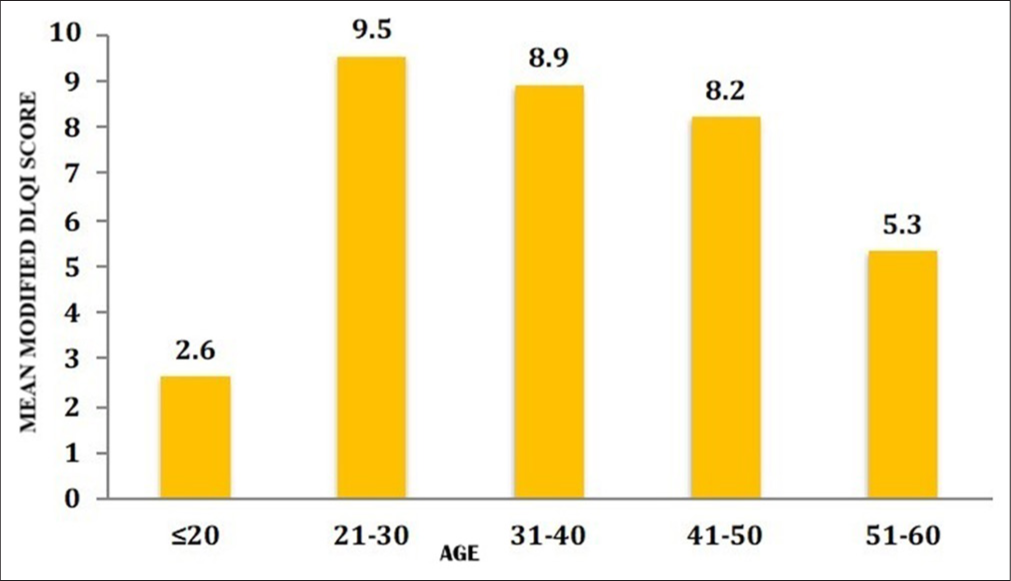
- Modified DLQI score variation with age.
Patients with fingernail involvement showed higher mean modified DLQI scores than patients with only toenail involvement (7.2 and 6.1, respectively). However, in patients with both finger and toe nails involved, a modified DLQI score of 7.5 was obtained, which was higher than each score. However, the difference was not statistically significant. Mean modified DLQI score showed variation with different nail conditions. The highest mean total score was found for paronychia (8.5) as compared to the overall mean score (6.9) [Table 4].
| Nail disorder | Mean total score |
|---|---|
| Onychomycosis | 6.4±5.2 |
| Paronychia | 8.5±4.1 |
| Ingrown toenail | 7.6±6.9 |
| Nail psoriasis | 7.1±6.6 |
| Idiopathic | 3.0±0.0 |
| Trachyonychia | 4.0±0.0 |
The final modified DLQI score obtained was calculated for each patient and grouped in the bands laid out, as shown in Figure 4. Various clinical cases and their modified DLQI scores are depicted in Figures 5-7.
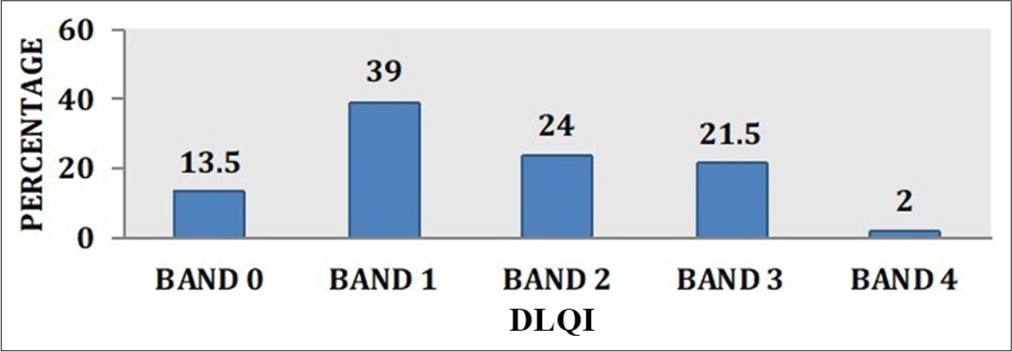
- Distribution of cases as per modified DLQI band.

- Nail psoriasis affecting all fingernails, modified DLQI score: 12.

- Onychomycosis of thumbnail, modified DLQI score: 13.

- Chronic Paronychia of right ring finger, modified DLQI score: 9.
DISCUSSION
Nail disorders contribute to nearly 10% of dermatologic consultations, substantially impacting patients’ QoL, especially through interference with daily function and cosmetic appearance.[8] In this study, we observed that onychomycosis was the most prevalent disorder, aligning with findings by Baran.[9] Onychomycosis and paronychia significantly impacted QoL, as indicated by their highly modified DLQI scores.
The study’s findings of a moderate DLQI impact, with a mean score of 6.9±5.5, parallels results of Reich and Szepietowski, who documented moderate QoL impairment in nail disorder patients.[2] Specifically, conditions such as acute paronychia, ingrown toenails and nail psoriasis, which induce pain and functional disruption, recorded higher scores, reflecting the acute effects on daily activities similar to the study by Belyayeva et al.[10]
Furthermore, demographic factors influenced QoL with younger age groups (particularly 21–30 years) reporting higher modified DLQI scores than older groups. This finding contrasts with studies that observed greater QoL impact in older patients, suggesting that younger individuals may face more social and professional pressures.[10,11] Gender also influenced QoL scores, with females recording higher scores than males (7.5 vs. 6.4), potentially due to heightened cosmetic concerns and cultural factors surrounding appearance, which has been noted similarly by previous studies.
Students and housewives had notably higher DLQI scores, attributable to the impact of nail disorders on academic and household tasks, respectively, while those in professional sectors reported lower scores, indicating less functional disruption in such roles. Interestingly, an inverted bell shaped pattern emerged regarding the number of nails involved and DLQI impact; higher scores occurred at both ends of the spectrum (1–5 nails and >10 nails), with a dip when 6–10 nails were affected. This could imply an adaptive tolerance when a moderate number of nails are impacted, while extensive involvement exacerbates distress, as seen in the previous studies.[12,13] In patients with only fingernail involvement, higher modified DLQI scores were reported as, fingernails often play a crucial role in daily activities. However, the score was even more when both fingers and toenails were affected.
This study emphasises the importance of using tools like the modified DLQI to assess the broader psychosocial and functional impact of nail disorders, particularly given their chronic and often visually apparent nature. By incorporating both quantitative and demographic insights, the modified DLQI can facilitate targeted interventions, addressing both medical and psychosocial aspects of nail disorders. Future research could validate these findings in larger, multi-centric cohorts.
CONCLUSION
Nail disorders are an important and understudied cause of impact on QoL of the patients. DLQI is a useful tool for assessment of QoL impact of a range of dermatological conditions. The use of a pre-validated modified DLQI questionnaire for application to nail disorders is unique. Considering the moderate impact of nail disorders on QoL, the usefulness and economic pliability of chronic and prolonged treatment choices for nail disorders can be concorded.
Authors’ contributions
All the authors’ contributed to the design, literature search, clinical studies, concepts, experimental studies, data acquisition, data analysis, statistical analysis and manuscript editing, preparation and reviewing.
Ethical approval
The research/study approved by the Institutional ethical approval no. 04/17 at Command Hospital Airforce Bangalore, dated 16th November 2017.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Sandeep Arora is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Development of the WHOQOL: Rationale and current status. Int J Ment Health. 1994;23:24-56.
- [CrossRef] [Google Scholar]
- Health-related quality of life in patients with nail disorders. Am J Clin Dermatol. 2011;12:313-20.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life and nail disorders. Acta Derm Venereol. 2007;87:255-9.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis: A study of self-recognition by patients and quality of life. Ind J Dermatol Venereol Leprol. 2015;81:270-74.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and treatment of nail disorders. Dtsch Arztebl Int. 2016;113:509-18.
- [CrossRef] [PubMed] [Google Scholar]
- Nail toxicities induced by systemic anticancer treatments. Lancet Oncol. 2015;16:181-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatology life quality index (DLQI)-a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-16.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines of care for nail disorders. J Am Acad Dermatol. 1996;34:529-33.
- [CrossRef] [PubMed] [Google Scholar]
- Baran and Dawber's diseases of the nails and their management (5th ed). Hoboken, NJ: Wiley Blackwell; 2019.
- [Google Scholar]
- The impact of nail disorders on quality of life. Eur J Dermatol. 2013;23:366-71.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life of persons with onychomycosis. Qual Life Res. 1993;2:341-48.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of toenail onychomycosis on patient quality of life. Int J Dermatol. 1997;36:754-6.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of onychomycosis on quality of life: Development of an international onychomycosis-specific questionnaire to measure patient quality of life. J Am Acad Dermatol. 1999;41:189-96.
- [CrossRef] [PubMed] [Google Scholar]