Translate this page into:
Adverse reaction to intralesional bleomycin therapy for periungual warts: A case report
*Corresponding author: K. Shilpa., Department of Dermatology, Bangalore Medical College, Bengaluru, Karnataka, India. shilpakvinod1980@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Narayan RV, Shilpa K, Grover C. Adverse reaction to intralesional bleomycin therapy for periungual warts: A case report. J Onychol Nail Surg. doi: 10.25259/JONS_16_2024
Abstract
Periungual warts pose a therapeutic challenge due to their persistence and proximity to the nail unit, which increases the risk of complications. Although conventional treatments exist, their efficacy is limited in this area. Intralesional bleomycin has emerged as an effective alternative, offering targeted cytotoxic effects. However, its use may be associated with potential adverse effects. This report presents an 18-year-old female with a verrucous plaque (2×3 cm) on the hyponychium and lateral nail folds. Intralesional bleomycin (0.1 mL of 3 U/mL) was administered after superficial paring. Post-injection, she developed severe pain, bluish-black discolouration, tense bullae and difficulty flexing the distal phalanx. Dermoscopy revealed pigment network, blue-grey clods and splinter haemorrhages. Arterial Doppler ruled out vascular compromise, and she was treated with nifedipine to enhance blood flow. The patient showed gradual improvement. Intralesional bleomycin is effective for periungual warts but requires a precise injection technique to avoid severe complications. Early recognition and management of adverse effects are critical to ensuring patient safety and treatment success.
Keywords
Periungual warts
Intralesional bleomycin
Adverse event
Nicolau syndrome
INTRODUCTION
Periungual warts, a common infection affecting the nail unit, present as a therapeutic challenge due to their persistence and potential for complications. While various treatment modalities exist, the efficacy of conventional options remains debatable in this location, necessitating the exploration of alternative approaches. Intralesional bleomycin, a cytotoxic agent, has emerged as a promising option, demonstrating targeted efficacy. Herein, we present the details of an 18-year-old female treated with intralesional bleomycin for a large periungual wart, emphasizing the potential adverse effects and their management.
CASE REPORT
An 18-year-old female presented with a long-standing verrucous plaque measuring 2×3cm involving the hyponychium, distal phalanx and lateral nail folds. The lesion, persisting for one year, exhibited bleeding on paring, prompting a clinical diagnosis of periungual wart [Figure 1a]. Intralesional bleomycin therapy was proposed considering the lesion’s extent and to prevent nail dystrophy. Following paring, intralesional injection of 0.1 mL of 3U/mL bleomycin solution was administered using a single puncture technique. The endpoint of injection was the appearance of blanching. Post-injection, the patient reported intense pain at the injection site and distal phalanx. The next day, she developed a bluish-black discolouration, with tense bullae over the proximal nail fold, along with a dusky mottled pigmentation over the distal phalanx. This was accompanied by difficulty in flexing the distal interphalangeal joint [Figure 1b]. Dermoscopy revealed the presence of an increased pigment network, blue-grey clods and splinter hemorrhages [Figure 1c].
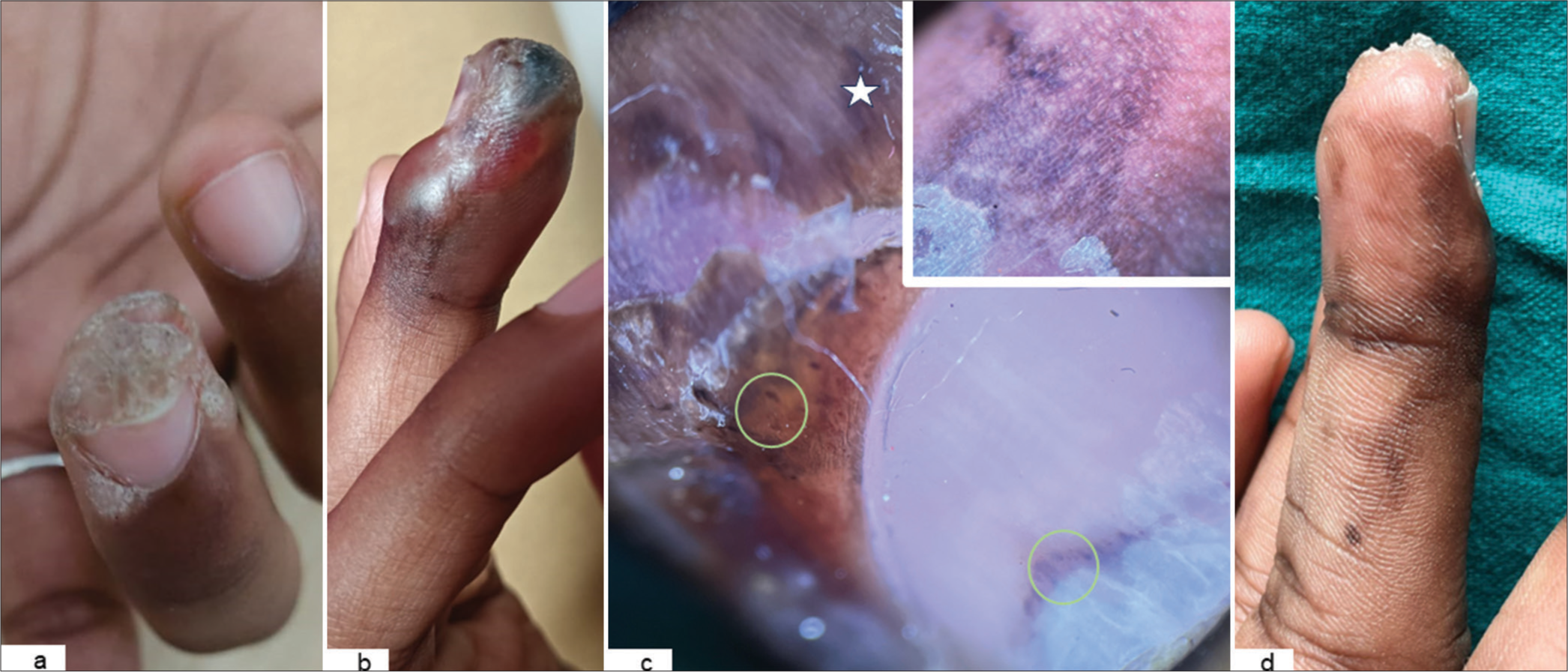
- (a) Baseline photograph showing the periungual wart. (b) Tense bullae over proximal and lateral nail fold with black eschar over the hyponychium. (c) Dermoscopy (DermLite DL100, Polarised×10) revealing the presence of splinter haemorrhages (yellow Circle) and blue-grey clods (star). Figure inset showing increased pigment network. (d) Four weeks follow-up showing residual hyperpigmentation of digit.
Due to the temporal correlation with bleomycin injection, a differential diagnosis of bleomycin extravasation-induced tissue necrosis and Nicolau syndrome was considered. The blister fluid was drained and sent for culture sensitivity, yielding sterile results. Arterial Doppler did not indicate any vascular compromise. Empirical antibiotic therapy with amoxicillin and clavulanic acid, with diclofenac and serratiopeptidase was initiated to prevent secondary infection. The patient was also initiated on nifedipine to improve the vascular supply to this acral area. Over 2 weeks, the patient reported reduction in pain and symptomatic relief. Initial difficulty in digit flexion gradually improved, with no persistent sensory deficit [Figure 1d].
DISCUSSION
Bleomycin has been reported to be an effective form of therapy for periungual warts; however, potential adverse effects, including perilesional hyperpigmentation, flagellate erythema, Raynaud’s phenomenon, tissue necrosis and gangrene, should always be kept in mind.[1] These adverse effects probably stem from its extended mechanism of action, as in addition to DNA damage, it causes haemorrhagic necrosis by inducing microthrombosis.[2] There have been earlier reports of digital necrosis following intralesional injection of bleomycin for warts, successfully treated with a combination of calcium channel blocker, aspirin and intravenous iloprost.[3] These call for careful attention to injection technique to prevent any extravasation of the drug into the surrounding normal tissue.
Various techniques for delivering bleomycin, including sublesional, translesional multipuncture and intralesional methods, have been employed. The translesional multipuncture approach involves the application of a droplet of the agent onto the wart surface, followed by puncturing with a lancet. This technique is favoured for its diminished pain compared to intralesional injection and potential for superior wart clearance outcomes.[4] Nevertheless, variations in the administered drug quantity and potential wastage may occur.[5]
The use of a bifurcated needle and the practice of paring are recommended to enhance the efficacy of bleomycin therapy. Needleless delivery methods, such as dermojet, exhibit limitations as they fail to penetrate lesions deeply enough, resulting in significant drug wastage. Emerging technologies, such as bleomycin-coated microneedle patches, offer promise in addressing the issue of drug wastage.[6]
A crucial consideration for both delivery techniques is the identification of injection endpoint, so as to prevent excessive drug administration. In the case of intralesional injection, the occurrence of well-defined blanching serves as a key endpoint. Conversely, for the translesional delivery technique, the occurrence of grey-white discolouration on the wart surface serves as a critical indicator. Understanding and adhering to these endpoints contributes towards optimising the therapeutic benefits of bleomycin while minimising the risk of unnecessary drug delivery.[7]
Nicolau syndrome or embolia cutis medicamentosa is a rare adverse effect of injectable therapy, characterised by blackish discolouration, livedo reticularis and tissue necrosis. It has been reported following intra- or peri-arterial injection of various medications. In a report by Nirmal et al., Nicolau syndrome was documented subsequent to the intralesional injection of 1% sodium tetradecyl sulphate for the treatment of pyogenic granuloma. The patient exhibited prompt blanching of the lesion immediately after injection, followed by the onset of a livedoid and bluish discolouration of the affected digit. Doppler study indicated a reduction in blood flow within the princeps pollicis artery. Management of the syndrome involved the administration of intravenous dipyridamole and subcutaneous heparin injections, as reported by them.[8] In another case encountered by Deshmukh et al., a similar manifestation of Nicolau syndrome was observed following the injection of 3% sodium tetradecyl sulphate for the treatment of pyogenic granuloma. Comparable to the previous case, the patient exhibited immediate blanching of the lesion post-injection, followed by a distinctive purplish discolouration of the affected digit.[9] Due to the early onset of similar changes in our patient, Nicolau syndrome was also kept as a possibility. An early diagnosis and prompt management, including the use of vasodilators, anticoagulants and supportive therapies, is pivotal for preventing irreversible tissue damage in this condition.
CONCLUSION
Intralesional bleomycin therapy for periungual warts, while offering a viable treatment option, demands careful consideration toward injection technique as well as potential adverse effects, including rare but severe complications such as Nicolau syndrome. Dermatologists undertaking this procedure should be well-versed in general precautions, making sure the drug stays within the lesion and be cautious of the amount injected. Recognising and promptly managing adverse events is imperative for ensuring patient safety and minimising long-term sequelae.
Authors’ contributions
Dr. Vignesh Narayan R: Data collection, draft manuscript preparation. Dr. Shilpa K : Study conception and design, Literature Review, Manuscript revision. Dr.Chander Grover: Manuscript revision, final manuscript preparation.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Chander Grover is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Efficacy and safety of intralesional bleomycin in the management of ungual warts. Skin Appendage Disord. 2020;6:346-50.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous toxicity of intralesional bleomycin administration in the treatment of periungual warts. Arch Dermatol. 1986;122:974-5.
- [CrossRef] [PubMed] [Google Scholar]
- Digital necrosis related to intralesional bleomycin. Eur J Intern Med. 2005;16:620.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional bleomycin injection vs microneedling-assisted topical bleomycin spraying in treatment of plantar warts. J Cosmet Dermatol. 2019;18:124-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of efficacy and safety of intralesional bleomycin in the treatment of common warts: Results of a pilot study. Indian J Dermatol Venereol Leprol. 2019;85:397-404.
- [CrossRef] [PubMed] [Google Scholar]
- Bleomycin therapy using multipuncture technique for resistant warts. Turk J Dermatol. 2019;13:91-3.
- [CrossRef] [Google Scholar]
- Gray-white discoloration of wart surface: An endpoint for multipuncture-assisted delivery of bleomycin. J Am Acad Dermatol. 2021;84:e227-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nicolau syndrome following sclerotherapy for pyogenic granuloma. Indian J Dermatol Venereol Leprol. 2014;80:484.
- [CrossRef] [PubMed] [Google Scholar]
- Nicolau syndrome following intralesional sclerotherapy: A dreaded complication of a simple office procedure. J Skin Stem Cell. 2020;7:e107198.
- [CrossRef] [Google Scholar]