Translate this page into:
Nail changes in dermatological diseases: A cross-sectional study at a tertiary care hospital
*Corresponding author: Bela Padhiar, Department of Dermatology, Gujarat Medical Education and Research Society Medical College, Gandhinagar, Gujarat, India. drbelapadhiar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Warke N, Padhiar B. Nail changes in dermatological diseases: A cross-sectional study at a tertiary care hospital. J Onychol Nail Surg. 2024;1:13-23. doi: 10.25259/JONS_2_2024
Abstract
Background:
The nail unit is involved in many skin and systemic diseases. Although easy to examine, this part is often not given due importance. For this, a deeper understanding of the various finer details of the nail changes is required. This knowledge can serve as a valuable addition to the clinical evaluation to arrive at an accurate clinical diagnosis.
Objectives:
The aim of this study was to assess the prevalence and spectrum of nail changes in patients with various dermatoses.
Material and Methods:
This was an observational, cross-sectional study conducted in the outpatient department of a tertiary care hospital. The sample size was calculated as 158. After Institutional Ethics Committee approval, patients were recruited by convenience sampling. Clinical examination and onychoscopy were done with photographic documentation after obtaining informed written consent. Descriptive statistics were applied for outcome variables, in the form of frequency and proportions.
Results:
A total of 163 patients (84 females and 79 males) were included in the study. The youngest patient was 1 year old, whereas the oldest was 78 years old. Dermatological disease seen in the study were clubbed into four major groups including infective (66 patients), inflammatory (64 patients), genodermatoses (10 patients), and miscellaneous (23 patients) disorders. The nail changes were divided into nail matrix, nail plate, nail bed, and nail fold changes. Onychomycosis was found to be the most common disease.
Conclusion:
Nail changes can provide valuable clinical insights, aiding clinicians in accurate diagnosis. Nails may provide evidence in support of diseases that may have occurred in the recent past, even though the skin manifestations may have resolved.
Keywords
Nail changes
Onychoscopy
Onycholysis
Subungual hyperkeratosis
Nail fold capillaroscopy
INTRODUCTION
The nail is a cutaneous appendage located on the distal phalanx of each digit.[1] The nail unit consists of a nail plate and four epithelia- the nail folds, nail matrix, nail bed, and hyponychium.[2] The nail unit can be involved in many systemic and skin diseases and may show changes specific to these conditions. Although easy to examine, nails are often not given its due importance. This study describes nail changes seen as an accompaniment of different dermatoses. It was aimed at assessing the prevalence and spectrum of nail changes seen among patients presenting with various dermatoses.
MATERIALS AND METHODS
This was an observational, cross-sectional study involving patients with nail changes presenting with various dermatological conditions to our outpatient dermatology clinic at a tertiary care hospital. Sample size at 95% confidence level was calculated by formula n= 4pq/d2 (p: 10% (from previous studies),[3] q: 1-p, d= clinical variation 5%). It was calculated as 144 and a 10% margin was added to make it a total of 158. The method of sampling used was convenience sampling. The study duration was 8 months. Approval from the Institutional Ethics Committee was taken prior to patient recruitment. Patients of all groups and both genders with nail changes were included in the study after informed consent. Inclusion criteria were patients with nail changes (either isolated nail changes or those in addition to dermatological disease). Those who refused to give consent for the study, or those who had applied henna or nail polish impairing visualisation of nail changes, were excluded from the study. A preset proforma was used to collect the patient’s details, including demographic data, detailed clinical history, and comorbidities. Clinical pictures of all nails were taken. Onychoscopy was done in conditions with established onychoscopic criteria in literature, to aid diagnosis. The findings were recorded, with photographic documentation. Instruments used for onychoscopy were Illuco IDS- 1100 (Illuco Co. Ltd, South Korea) (polarised light for nail bed changes, non-polarised light for nail plate changes) and Dino-Lite AM3111 (AnMo corporation, Taiwan) for nail fold videocapillaroscopy (polarised light). Relevant investigations were carried out when the diagnosis was not clear clinically. For analysis, nail changes seen were divided into four major categories, namely, infective disease, inflammatory or autoimmune disease, genodermatoses, and miscellaneous disorders. Descriptive statistics were calculated in the form of frequency and proportions to evaluate outcome variables.
RESULTS
The duration of the study was 8 months (November 2022– June 2023). Overall, 163 patients were enrolled. The youngest patient was 1 year old, whereas the oldest was 78 years old. Maximum patients belonged to the 31–40 years age group. Mean age was 40.528 ± 17.128 years at 95% confidence interval. Our study includes 84 females and 79 males.
Of these, 66 had infectious diseases, 64 had inflammatory or autoimmune diseases, 10 had genodermatoses, and 23 belonged to the miscellaneous category. Nail changes seen in different diseases are summarised in Tables 1 and 2. Notable features are mentioned below.
| Disease | Nail plate findings | Nail matrix findings | Nail bed findings | Nail fold findings | ||||
|---|---|---|---|---|---|---|---|---|
| Feature | N (%) | Feature | N (%) | Feature | N (%) | Feature | N (%) | |
| Infective diseases (n=66) | ||||||||
| Onychomycosis (n=52) | Chromonychia | 23 (44) | Onychomadesis | 4 (8) | Onycholysis | 37 (71) | Paronychia | 4 (8) |
| Leukonychia | 3 (6) | Pits | 1 (2) | Subungal hyperkeratosis | 17 (33) | |||
| Ridging of nail plate | 1 (2) | Dystrophy | 7 (13) | |||||
| Thickening of nails | 3 (6) | Anonychia | 1 (2) | |||||
| Longitudinal melanonychia | 1 (2) | |||||||
| Hand foot mouth disease (n=2) | Onychomadesis | 2 (100) | ||||||
| Paronychia (n=7) | Acute paronychia | 7 (100) | ||||||
| Warts (n=5) | Verrucous growth in nail bed | 1 (20) | Verrucous growth in nail fold | 5 (100) | ||||
| Onycholysis | 1 (20) | |||||||
| Inflammatory and autoimmune diseases (n=64) | ||||||||
| Erythroderma (n=2) | Thickening | 1 (50) | Dystrophy | 2 (100) | Subungual hyperkeratosis | 2 (100) | Paronychia | 2 (100) |
| Overcurvature of nails | 1 (50) | Onychomadesis | 1 (50) | |||||
| Beau's lines | 1 (50) | |||||||
| Lichen planus (n=4) | Thinning of nail plate | 2 (50) | Onychomadesis | 1 (25) | ||||
| Ridging | 3 (75) | Pterygium | 2 (50) | |||||
| V-shaped nicking | 1 (25) | |||||||
| Trachyonychia | 1 (25) | |||||||
| Psoriasis (n=19) | Exogenous chromonychia | 1 (5) | Pitting | 16 (80) | Onycholysis | 15 (75) | Inflammation | 1 (5) |
| Thickening | 1 (5) | Dystrophy | 1 (5) | Subungual hyperkeratosis | 4 (20) | |||
| Leukonychia | 1 (5) | Beau’s lines | 2 (10) | Salmon patch | 1 (5) | |||
| Melanonychia | 1 (5) | Anonychia | 1 (5) | |||||
| Trachyonychia | 1 (5) | |||||||
| Alopecia areata (n=2) | Pitting | 2 (100) | ||||||
| Pemphigus vulgaris (n=2) | Thickening | 1 (50) | Dystrophy | 1 (50) | ||||
| Yellowish discolouration of nails | 1 (50) | Onychomadesis | 1 (50) | |||||
| Beau's lines | 1 (50) | |||||||
| Eczema (n=24) | Ridging | 5 (21) | Dystrophy | 1 (4) | Subungual hyperkeratosis | 2 (8.5) | Eczema of nail fold | 13 (54.16) |
| V shaped nicking | 1 (4) | Beau's lines | 1 (4) | Onycholysis | 2 (8.5) | |||
| Onychoschizia | 3 (12.5) | Onychomadesis | 2 (8.5) | |||||
| Exogenous chromonychia | 2 (8.5) | |||||||
| Thinning | 3 (12.5) | |||||||
| Fissuring | 1 (4) | |||||||
| Median canaliform dystrophy | 1 (4) | |||||||
| Longitudinal melanonychia | 1 (4) | |||||||
| Systemic sclerosis (n=6) | Dystrophy | 1 (17) | Mizutani's finger pad sign | 1 (17) | Resorption of digits | 4 (67) | ||
| Tapering of digits | 1 (17) | |||||||
| Pitted scars scleroderma | 1 (17) | |||||||
| Subacute lupus erythematosus (n=2) | Paronychia | 1 (50) | ||||||
| Dermatomyositis (n=1) | Erythema of nail fold | 1 (100) | ||||||
| Genodermatoses (n=10) | ||||||||
| Darier's disease (n=3) | V shaped nicking | 2 (67) | Nail dystrophy | 1 (33) | Subungual hyperkeratosis | 1 (33) | ||
| Longitudinal melanonychia | 1 (33) | |||||||
| Erythronychia | 1 (33) | |||||||
| Epidermolysis bullosa (n=2) | Pterygium | 1 (50) | Onycholysis | 1 (50) | ||||
| Dystrophy | 2 (100) | |||||||
| Onychomadesis | 1 (50) | |||||||
| Palmoplantar keratoderma (n=2) | Ridging | 1 (50) | Nail fold desquamation | 1 (50) | ||||
| Dystrophy | 1 (50) | Conical tapering of fingers | 1 (50) | |||||
| Tuberous sclerosis (n=2) | Fibroma | 2 (100) | ||||||
| Apert syndrome (n=1) | Syndactyly | 1 (100) | ||||||
| Miscellaneous disorders (n=23) | ||||||||
| Nutritional dermatoses (n=5) | Ridging | 2 (40) | Dystrophy | 2 (40) | ||||
| Koilonychia | 2 (40) | Onychomadesis | 1 (20) | |||||
| Onychoschizia | 1 (20) | |||||||
| Thinning of nail plate | 1 (20) | |||||||
| Whitening and hardening of all nails | 1 (20) | |||||||
| Chromonychia (n=5) | Endogenous chromonychia (brown) | 1 (20) | Blue lunulae | 1 (20) | ||||
| Exogenous chromonychia (brown) | 2 (40) | Leukonychia | 1 (20) | |||||
| Cryptonychia (n=3) | Incurving of nail plate | 3 (100) | ||||||
| Granulation tissue | 2 (67) | |||||||
| Trauma (n=4) | Pterygium | 1 (25) | Onycholysis | 1 (25) | ||||
| Haematoma | 2 (50) | |||||||
| Fibrokeratoma (n=2) | Subungual fibrokeratoma | 1 (50) | Periungual fibrokeratoma | 1 (50) | ||||
| Disease | Nail change | Percentage | Number of patients |
|---|---|---|---|
| Psoriasis (n=19) | |||
| Pitting | 90 | 18 | |
| Onycholysis | 75 | 15 | |
| Compact subungual hyperkeratosis | 20 | 4 | |
| Systemic sclerosis (n=6) | |||
| Microhemorrhages | 17 | 1 | |
| Dilated capillaries | 34 | 2 | |
| Capillary drop out | 17 | 1 | |
| Avascular areas | 67 | 4 | |
| Subacute cutaneous lupus erythematosus (n=2) | |||
| Dilated capillaries | 50 | 1 | |
| Dermatomyositis (n=1) | |||
| Bushy capillaries | 100 | 1 | |
| Onychomycosis (n=52) | |||
| Longitudinal spike pattern | 75 | 39 | |
| Aurora borealis pattern | 37 | 19 | |
| Ruin pattern | 12 | 6 | |
Infective diseases
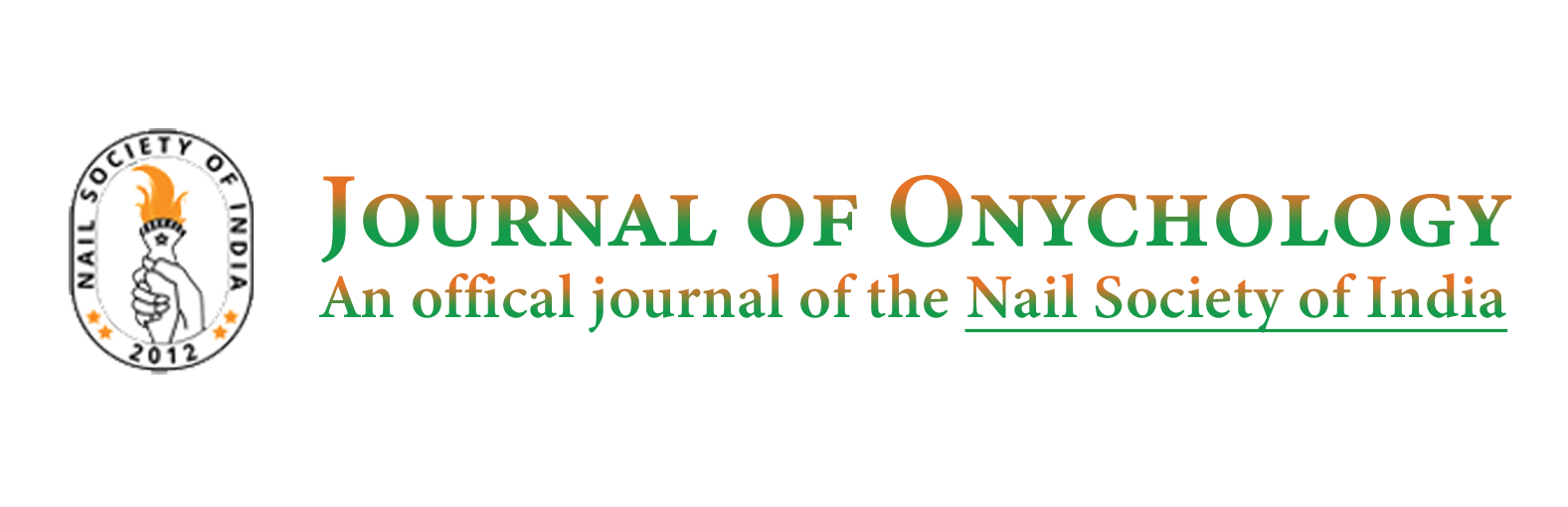
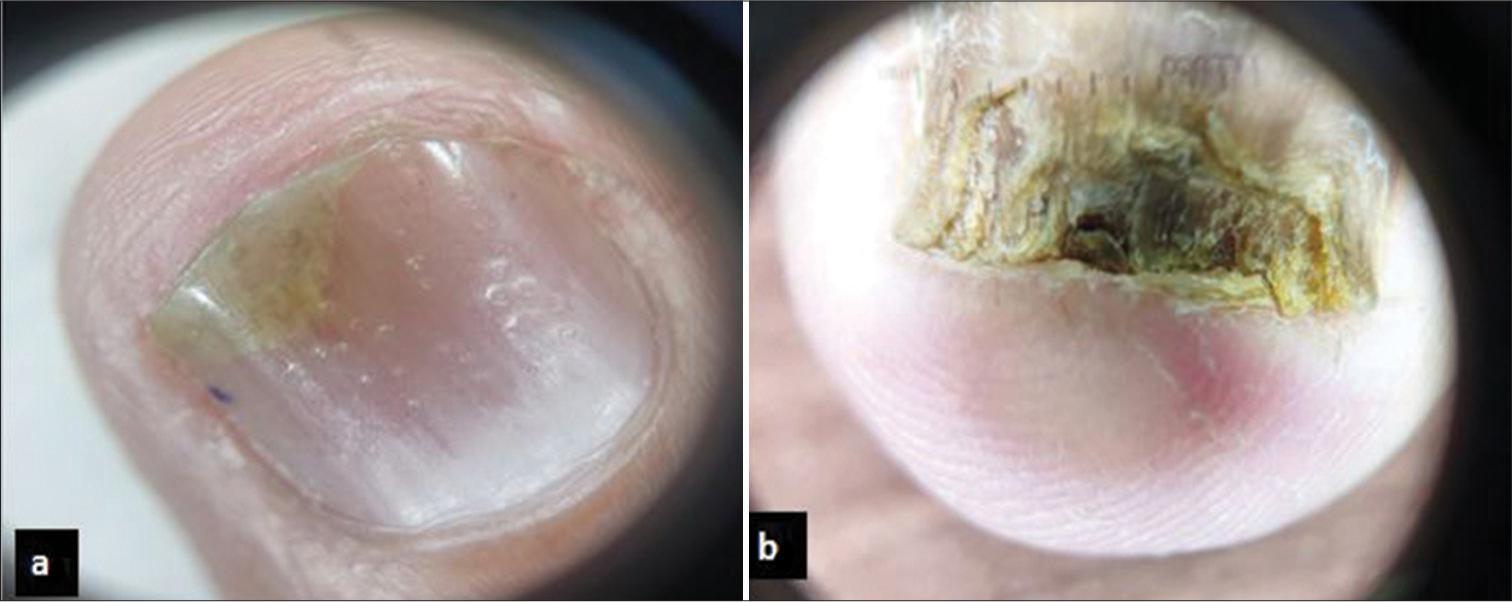
Onychomycosis was the most common infective as well as commonest nail disease overall (67% of cases). The nail changes seen were chromonychia in 24 (44%) patients seen as brown to black colour, and leukonychia in 3 (6%) patients have [Figure 1a]. Acute Paronychia was commonly seen in females, and the right hand was the most commonly affected. Periungual warts were seen in five patients. Onycholysis was seen in one case due to a wart in the nail bed region [Figure 1b]. Nail changes with hand-foot-mouth disease were seen in two patients, both presenting with onychomadesis. Onychoscopy of onychomycosis showed longitudinal spike pattern, aurora borealis pattern and ruin pattern [Figure 2].

- (a) White superficial onychomycosis of toenails and (b) periungual wart on nail bed on finger nail showing onycholysis.

- (a) Onychoscopic image of onychomycosis showing chromonychia and longitudinal spike pattern (Illucco IDS 1100, × 10, polarised). (b) Onychoscopic image showing friable subungual hyperkeratosis or ruin pattern in onychomycosis (Illucco IDS 1100, ×10, polarised).
Inflammatory/Autoimmune diseases
Out of 20 patients with psoriasis, affecting the nail matrix, pitting was the most frequent change seen [Figures 3 and 4]. Nail changes in alopecia areata were seen in two patients in the form of regular pitting [Figure 5a]. Out of four patients with lichen planus, nail changes such as thinning, ridging, v-shaped nicking, pterygium, and onychomadesis were seen [Figure 5b]. Nine patients with autoimmune connective tissue diseases were included [Figures 6-8]. In two patients with pemphigus vulgaris, the nail changes observed were thickening, yellowish discoloration, nail dystrophy, onychomadesis, and Beau’s lines. Two patients of erythroderma were included in our study. One was secondary to photodermatitis (eczematous dermatitis), and one was secondary to psoriasis. In patients with eczema, the most common nail change seen was eczema of the nail fold.

- (a) Coarse pits, onycholysis of nail plate and erythematous plaques with scaling of nail folds. (b) Trachyonychia of nail (rough type) in psoriasis.
- (a) Onychoscopic image showing coarse irregular pitting and onycholysis in psoriasis. (Illucco IDS 1100, ×10, polarised) (b) Onychoscopic image of subungual compact hyperkeratosis in psoriasis (Illucco IDS 1100, ×10, polarised).

- (a) Fine, regular pitting in alopecia areata. (b) Pterygium secondary to lichen planus.

- (a) Pitted scars on finger pad (Early stage of scleroderma). (b) Resorption of tuft of fingers (late stage of scleroderma).

- (a) Onychoscopic image of microhaemorrhages (black circle) on proximal nail fold capillaroscopy in active stage of scleroderma (Dino-Lite AM3111, polarised, ×2060) and (b) onychoscopic image of avascular areas (black arrow) in proximal nail fold in late stage of scleroderma (Dino-Lite AM3111, polarised, ×200).

- (a) Onychoscopic image of systemic lupus erythematosus showing meandering capillaries (white circle) (Dino- Lite AM3111, polarised, × 200) and (b) Onychoscopic image showing bushy capillaries in dermatomyositis (black circle) (Dino-Lite AM3111, polarised, × 200).
Genodermatoses
Patients with genodermatoses included in our study were Darier’s disease, Apert syndrome [Figure 9a], palmoplantar keratoderma (PPK), tuberous sclerosis [Figure 9b] and epidermolysis bullosa (EB). Apert syndrome is a rare genodermatosis with dysmorphic facies, syndactyly of fingers and toes.

- (a) Syndactyly in Apert syndrome and (b) fibrokeratoma on finger nail in a patient having angiofibromas on face (case of tuberous sclerosis).

- (a) Subungual fibrokeratoma on finger nail and (b) cryptonychia of toe nail.
Miscellaneous disorders
Among nail dyschromias, melanonychia was the most frequently observed change. Other types of chromonychia noted included both brown endogenous and exogenous chromonychia, as well as blue lunulae.
Out of four patients having nail changes secondary to trauma, two patients had a subungual hematoma, one had traumatic onycholysis, and one had traumatic pterygium. Two patients of fibrokeratoma (nail bed and proximal nail fold) were included in our study [Figure 10a]. Out of three patients with onychocryptosis, two patients had granulation tissue at the nail fold and incurving of the nail plate [Figure 10b]. Among patients presenting with nutritional deficiency related dermatoses, nail plate changes seen were ridging, koilonychia, thinning of the nail plate, and whitening and hardening of all the nails. Nail matrix changes included dystrophy and onychomadesis.
DISCUSSION
Nail changes account for 10% of all dermatological conditions.[3] In the present study, among a total of 163 patients, onychomycosis (52 patients) was the most common nail disease. These findings are consistent with other studies.[4-7]
Infective diseases
Among the cases of onychomycosis, distal lateral subungual onychomycosis was the most common type, which is in concordance with other studies.[4-7] Pitting was seen in one patient with onychomycosis, which was not found in the above quoted studies. Pitting is reported to be a rare finding in onychomycosis.[8] Other features we saw, were in concurrence with the study by David et al.[4]; however, additional findings which they reported included Beau’s lines and greenish discolouration.[4] Onychoscopic changes suggestive of onychomycosis in the form of spiked and jagged edges, ‘Aurora borealis’ pattern, and subungual ‘ruins’ pattern (65%) were seen in 18 (90%), 17 (85%) and 13 (65%) patients, respectively, by Ankad et al.[9] Other findings including lamellar microsplitting and defined patterns of leukonychia, reported in some studies[10,11], were not visualised in our cases. Regarding acute paronychia, our study had a male-to-female ratio of 1:5, similar to the report by Rani et al.[6] The right hand was found to be affected more often, similar to other studies.[6,7] This could be because of the longer duration of contact with water.
Patients with hand-foot-mouth disease have been reported to develop nail findings in the form of Beau’s lines, onychomadesis, yellowish discolouration of nail plate, and leukonychia.[12] These changes resolve spontaneously after 8 weeks.[13] Five patients with periungual warts in our study was a higher proportion as compared to previous study by David et al.[4], who reported warts in one patient out of 550 patients; or Rathi et al.[7] who reported nine patients among 225 patients. This difference is probably due to the varying prevalence of this infectious condition.
Inflammatory/autoimmune conditions
Table 3 compares the findings in our study with other studies of nail changes in psoriasis. Onychoscopic findings of pitting, onycholysis, and subungual hyperkeratosis were seen in 90%, 75% and 20% cases, respectively. Similar results were reported in previous studies.[14,15] Onycholysis may occur due to multiple reasons. Most common causes of onycholysis include nail psoriasis and onychomycosis, followed by less common causes including trauma and warts. In psoriasis, the onycholysis frequently has an erythematous border at its proximal edge. In onychomycosis, the onycholysis has a jagged proximal edge.[9] Differentiating between nail psoriasis and onychomycosis may be clinically tricky at times. Onychoscopy may come in handy at such times. The prevalence of onychomycosis is higher in patients with psoriasis than in the general population. Furthermore, both conditions may coexist. Thus, clinically, psoriasis patients whose nails appear resistant to treatment should be evaluated for onychomycosis by relevant investigations.[16].
| Nail change | Our study (n=20) (%) | Rathi et al.[7] (n=26) (%) | David et al.[4] (n=161) (%) | Kumar et al.[5] (n=82) (%) |
|---|---|---|---|---|
| Pitting | 80 | 88.46 | 100 | 30.4 |
| Discolouration | - | 76.92 | 2.48 | 8.53 |
| Subungual hyperkeratosis | 20 | 23 | 87.57 | 21.9 |
| Onycholysis | 75 | 23 | 4.96 | 10.9 |
| Ridging | - | 69.23 | 97.56 | |
| Oil drop sign | 5 | - | 11.80 | 8.53 |
| Parrot beaking | - | - | 0.62 | |
| Beau’s lines | 10 | - | 1.86 | 9.75 |
| Dystrophy | 5 | - | 50.31 | 9.75 |
| Splinter haemorrhage | - | - | 6.21 | 8.53 |
Rathi et al., had reported one patient with alopecia areata in their series, presenting with nail pitting.[7] In the study by Rani et al., pitting was seen in 64% of patients.[6] In the study conducted by David et al., superficial pits in a scotch plaid pattern were seen in all patients with alopecia areata.[4] Nail involvement in alopecia areata is commonly seen in children or in those with severe forms of alopecia. Pitting is a common feature, presenting as a fine and geometric pattern in alopecia areata, in contrast to the coarse pits seen in psoriasis. Nail involvement is considered a poor prognostic marker in alopecia areata. Thus, their presence and assessment of severity may guide management decisions. Nail changes often occur simultaneously with hair loss but may precede or follow hair changes.[17]
Table 4 compares the findings in nail lichen planus in our study with other similar studies. Longitudinal ridging, fissuring, nail plate thinning, and trachyonychia were common findings in nail lichen planus. Melanonychia is the most common finding in some studies which was not observed in our study.[18]
| Nail change | Our study (n=4) (%) | Rathi et al.[7] (n=26) (%) | David et al.[4] (n=22) (%) | Kumar et al.[5] (n=50) (%) |
|---|---|---|---|---|
| Thinning of nail plate | 50 | 75 | - | 10 |
| Longitudinal striations | 75 | 75 | 4.54 | 52 |
| Trachyonychia | 25 | - | 9.09 | 10 |
| Melanonychia | - | 25 | 4.54 | 6 |
| Pterygium | 50 | 25 | 18.1 | 8 |
| Dystrophy | - | - | 22.72 | 8 |
| Beau’s lines | - | - | - | 6 |
| Pits | - | 12.5 | 13.63 | - |
| Anonychia | - | - | 4.54 | - |
| Onychoschizia | - | - | 13.63 | - |
| V shaped nicking | 25 | - | - | - |
| Onychomadesis | 25 | - | - | - |
Trachyonychia is a disorder of the nail unit that most commonly presents with rough, longitudinally ridged nails (opaque trachyonychia) or, less frequently, with uniform, opalescent nails with pits (shiny trachyonychia). The rough type is considered to be the more severe type. Dermatologic conditions commonly associated with trachyonychia include alopecia areata/alopecia universalis, lichen planus, and psoriasis.[19]
There are both clinical as well as dermoscopic changes in autoimmune connective tissue disorders. Scleroderma presents as a shortening of fingers, fingertip scars, digital necrosis, pseudo-clubbing, and ragged cuticles as prominent clinical changes.[7,20] Nail fold capillaroscopic changes are primarily divided into three patterns signifying early, active, and late disease, as described by Grover et al.[21] Clinical nail changes in lupus erythematosus include onycholysis, discolouration, longitudinal ridging, nail fold erythema, etc.[20] Nail-fold capillaroscopy anomalies are detected less frequently and less consistently in systemic lupus erythematosus. Extremely lengthy capillary loops (>750 m), meandering capillaries, and a large subpapillary venous plexus are the most commonly reported anomalies.[21] Clinical nail changes seen in dermatomyositis include ragged cuticles and erythema of the nail fold. Apart from systemic sclerosis, dermatomyositis has the most consistent nail-fold capillaroscopy abnormalities.[22] Increased micro haemorrhages and elongated capillaries are well correlated with myalgia and arthralgia, respectively. Avascular areas and budding or bushy capillaries, which suggest ischemia and revascularisation, respectively, are observed most frequently in dermatomyositis.[22]
In pemphigus vulgaris, nail manifestations include paronychia, Beau’s lines, onycholysis, subungual haemorrhages and onychomadesis. The type and onset of nail changes may reflect varying severity of the disease. Nail involvement frequently occurs before or with a flare of disease and is rarely a part of the initial presentation.[23] Thus, nail involvement in pemphigus warrants attention as it may serve as a harbinger of the flare-up of disease or severe disease, thus warranting aggressive systemic treatment. The resolution of nail diseases takes longer than resolution of skin manifestations.[24]
In erythroderma, nail changes commonly observed are shiny nails, subungual hyperkeratosis, longitudinal ridging, onycholysis, nail dystrophy, Beau’s lines, and onychomadesis.[6,7] Nail changes are most commonly seen in psoriatic erythroderma, as per the study by Mathew and Sreedevan.[25] Nail changes can act as a pointer to the causative disease like psoriasis.[6]
Nail changes seen in eczema in various studies include onycholysis, ridging, subungual hyperkeratosis, and pitting.[4-7] Nail changes in eczema are more frequent in patients who have lesions on the hand and foot; this indicates that the involvement of the nail bed or matrix in continuity with the skin on hands and feet may result in nail changes.
Genodermatoses
Darier’s disease frequently presents as longitudinal red and white bands, V-shaped nicking of fingernails, nail dystrophy, etc.[4-7] These features are not exclusive to Darier’s disease, but can provide valuable clues for diagnosis.
Apert syndrome is a rare entity. With only a few cases reported in the literature, our case would be instrumental in adding to the existing pool of data.
In tuberous sclerosis, fibromas or Koenen’s tumours appear during puberty and are present in 50% of cases.[26] In a study by Liebman et al., 61 patients had ungual fibromas. About half of the patients with ungual fibromas had both periungual and subungual lesions, with periungual fibromas predominating overall. Periungual fibromas were seen as pink papules originating from under the proximal or lateral nail fold. The underlying nail plate had a longitudinal groove.[27]
Nail involvement is one of the earliest symptoms of EB and can occur even before skin blistering. In EB simplex, onychomadesis and onycholysis can occur in severe subtypes, whereas in junctional and dystrophic forms, nail changes are closely associated with the severity of the disease. In these subtypes, nail involvement is in the form of loss of nails in severe forms and onycholysis and dystrophy in milder forms.[28] Rathi et al. also found two patients with EB where the nails were dystrophic in both patients and onycholysis was seen in one patient. Both patients had finger nail involvement. None of these had any history of skin or systemic disease.[7] It is in contrast to our cases where one patient had haemorrhagic blisters on the skin.
PPKs are sometimes present with nail abnormalities. Pachyonychia congenita typically presents with toenail dystrophy, focal keratoderma and plantar pain. David et al. had also reported one patient of PPK with nail changes.[4] In study by Rani et al., three cases were PPK, with thickening, discoloration, and Beau’s lines involving nails were reported.[6] The findings seen in our patients were ridging, and dystrophy.
Miscellaneous
Nail dyschromias are often a cause of concern to patients. It represents a colour difference in the material or the surface of the nail plate or subungual tissue. The most prevalent type of nail dyschromia is leukonychia, which is an opaque white staining of the nail. There are three forms of leukonychia: true leukonychia, apparent leukonychia and pseudoleukonychia. Melanonychia is a black-brown darkening of the nail caused by melanin deposition. There are three types of melanonychia: longitudinal, diffuse and transverse. Blue chromonychia is most commonly attributable to drug use (including antimalarials, chemotherapeutic agents and azidothymidine). Additional causes include exposure to silver salts, Wilson’s disease, glomus tumour of the nail and digital malformations. Other types of chromonychia are also seen (yellow, red or green types).[29,7]
In our study, melanonychia was found as an isolated finding in six patients, and in conjunction with other findings (such as Darier’s disease and onychomycosis) in a number of patients. Nail dyschromia occurs due to many causes and we found five patients with isolated nail chromonychia, namely, three dark brown, one blue discolouration of lunulae, and one punctate leukonychia.
Another aspect of chromonychia is that they may be due to endogenous or exogenous causes. The exogenous chromonychia has a proximal margin parallel to the margin of the proximal nail fold, whereas the endogenous chromonychia is parallel to the convex margin of the lunula.[4,7,30]
The nail changes may be associated with occupation. A patient with traumatic pterygium who was a farmer by occupation, and another with onycholysis who was a carpenter, were noted. We found two cases of subungual hematoma of the nail bed secondary to trauma. While it is a benign and self-resolving condition, it may sometimes be confused with more sinister diagnoses like subungual melanoma.
Onychocryptosis was seen in three cases in our study. In the study by Rathi et al., it was found in one patient (0.4%),[7] whereas in the study by David et al., it was found in 11 (2%) patients.[4] In a study by Rani et al., six patients were found to have ingrown toenails (3.77%).[6]
A study by Palaniappan et al. that described the demographic and clinical characteristics of fibrokeratoma found that most lesions occur on the fingers with the dorsal involvement being more common.[31] In our study, we found a subungual fibrokeratoma, which is a rare finding and a dorsal finger fibrokeratoma, which is common.[32]
In our study, koilonychia was seen in two patients similar to other studies.[4,6,7] Dystrophy was seen in two patients and onychomadesis was seen in one patient. Onychoschizia, ridging, thinning and hardening of nail plate were the other changes seen. Nutritional changes in nails provide clues to underlying deficiencies when other signs may not be evident. Due to their relatively slower rate of regeneration as compared to the skin, nails provide evidence of any disease that may have occurred in the recent past when the skin manifestations have disappeared.
CONCLUSION
Nail manifestations of many diseases may appear similar when observed superficially. However, a deeper knowledge of characteristics can help one identify the unique characteristics of nail changes in some dermatoses.
Authors’ contributions
Concept- Padhiar B, design- Warke N and Padhiar B, the definition of intellectual content- Padhiar B and Warke N, literature search- Warke N, data acquisition- Padhiar B, data analysis- Warke N, statistical analysis- Padhiar B, manuscript preparation- Warke N, manuscript editing- Padhiar B, and manuscript review- Padhiar B. Guarantor- Padhiar B and Warke N.
Ethical approval
The research/study was approved by the Institutional Review Board at Institutional Ethics Committee, GMERS Medical College, Gandhinagar, number GMERS/MCG/IEC/25/2022, dated 12 October 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Fitzpatrick’s dermatology (9th ed). United States of America: McGraw-Hill Education; 2019. p. :106-7.
- [Google Scholar]
- Structure and function of the skin In: Grifftiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook’s textbook of dermatology (9th ed). West Sussex, UK: John Wiley and Sons, Ltd; 2016. p. :2.9-10.
- [Google Scholar]
- Nail findings: What is a provider to do? Physician Assist Clin. 2016;1:347-61.
- [CrossRef] [Google Scholar]
- Nail abnormalities associated with various dermatoses in a tertiary care center in North India: A cross-sectional study. J Dermatol Dermatol Surg. 2021;25:119-23.
- [CrossRef] [Google Scholar]
- Nail changes in various dermatoses: An observational study conducted at tertiary care center, Ujjain, Madhya Pradesh, India. Int J Res Dermatol. 2020;6:237-43.
- [CrossRef] [Google Scholar]
- Study of nail disorders in dermatology. Int J Contemp Med Res. 2019;6:A1-6.
- [CrossRef] [Google Scholar]
- A prospective study of nail changes in dermatological and systemic illnesses. Ann Int Med Dent Res. 2018;4:DT5-11.
- [CrossRef] [Google Scholar]
- Nail psoriasis: Clinical features, pathogenesis, differential diagnoses, and management. Psoriasis (Auckl). 2017;7:51-63.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of onycholysis due to nail psoriasis, onychomycosis and trauma: A cross sectional study in skin of color. Indian Dermatol Online J. 2020;11:777-83.
- [CrossRef] [PubMed] [Google Scholar]
- Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2013;27:509-13.
- [CrossRef] [PubMed] [Google Scholar]
- Nail dermoscopy (onychoscopy) findings in the diagnosis of primary onychomycosis: A cross-sectional study. Indian J Dermatol Venereol Leprol. 2020;86:341-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nail changes in hand-foot-and-mouth disease (HFMD) Indian Dermatol Online J. 2021;12:656-7.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical study of nail changes occurring secondary to hand-foot-mouth disease: Onychomadesis and beau's lines. Ann Dermatol. 2014;26:280-3.
- [CrossRef] [PubMed] [Google Scholar]
- A dermoscopic study of nail involvement in chronic plaque psoriasis at a tertiary care center. Asian J Med Sci. 2022;13:101-6.
- [CrossRef] [Google Scholar]
- Dermoscopic features of nail psoriasis: An observational, analytical study. Skin Appendage Disord. 2020;6:207-15.
- [CrossRef] [PubMed] [Google Scholar]
- Fungal infections and nail psoriasis: An update. J Fungi (Basel). 2022;8:154.
- [CrossRef] [PubMed] [Google Scholar]
- Alopecia areata of the nails: Diagnosis and management. J Clin Med. 2024;13:3292.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features and treatment outcomes of nail lichen planus: A retrospective study. JAAD Case Rep. 2021;17:43-4.
- [CrossRef] [PubMed] [Google Scholar]
- Trachyonychia: Review and update on clinical aspects, histology, and therapy. Skin Appendage Disord. 2016;2:109-15.
- [CrossRef] [PubMed] [Google Scholar]
- Nail changes in connective tissue diseases: A study of 39 cases. Pan Afr Med J. 2014;18:150.
- [CrossRef] [PubMed] [Google Scholar]
- Nail-fold capillaroscopy for the dermatologists. Indian J Dermatol Venereol Leprol. 2022;88:300-12.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillaries in connective tissue diseases in skin of color: A dermoscopic view. Clin Dermatol Rev. 2019;3:115-20.
- [CrossRef] [Google Scholar]
- Nail changes in pemphigus and bullous pemphigoid: A single-center study in China. Front Med (Lausanne). 2022;9:933608.
- [CrossRef] [PubMed] [Google Scholar]
- Nail involvement in autoimmune bullous disorders. Dermatol Clin. 2011;29:511-3.
- [CrossRef] [PubMed] [Google Scholar]
- Erythroderma: A clinicopathological study of 370 cases from a tertiary care center in Kerala. Indian J Dermatol Venereol Leprol. 2017;83:625.
- [CrossRef] [PubMed] [Google Scholar]
- Koenen tumors in tuberous sclerosis: A review and clinical considerations for treatment. Ann Plast Surg. 2014;73:721-2.
- [CrossRef] [PubMed] [Google Scholar]
- Nail involvement in epidermolysis bullosa. Dermatol Clin. 2010;28:153-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nail dyschromias. Indian J Dermatol Venereol Leprol. 2011;77:652-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nail disorders In: Sacchidanand S, Somaiah S, Kanathur S, Kumar S, eds. IADVL textbook of dermatology (5th ed). Mumbai: Bhalani Publishing House; 2022. p. :1899.
- [Google Scholar]
- Acquired fibrokeratoma: A retrospective study in a tertiary centre in South India. Indian J Dermatol. 2022;67:312.
- [CrossRef] [PubMed] [Google Scholar]
- Tumors of the nail apparatus and adjacent tissues In: Baran R, Berker D, Holzberg M, Piraccini B, Thomas L, eds. Baran's and Dawber's diseases of the nails and their management (5th ed). United States: John Wiley and Sons, Ltd; 2019. p. :712.
- [CrossRef] [Google Scholar]