Translate this page into:
Squamous cell carcinoma of nail unit masquerading as pyogenic granuloma
*Corresponding author: Ishika Muradia, Department of Dermatology and STD, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. ishikathedermatologist.13@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Muradia I, Bansal S, Sharma S. Squamous cell carcinoma of nail unit masquerading as pyogenic granuloma. J Onychol Nail Surg. doi: 10.25259/JONS_6_2024
Abstract
Squamous cell carcinoma (SCC) of a nail unit is an uncommon tumour with low metastatic potential. These tumours are commonly misdiagnosed due to their variable presentation. We report a case of a 53-year-old female presenting with a solitary, painless growth with bleeding tendency, present over her right index finger, persisting for 4 years. Histopathological examination confirmed the diagnosis of SCC. This report aims to highlight the clinical presentation, diagnostic approach and treatment of SCC in an unusual location, emphasising the importance of early detection and management.
Keywords
Nail unit
Squamous cell carcinoma
Masquerading
Pyogenic granuloma
INTRODUCTION
Squamous cell carcinoma (SCC) of the nail unit is uncommon.[1] It can have a very non-specific presentation, resembling benign inflammatory and infective conditions such as paronychia, pyogenic granuloma and verruca vulgaris, to name a few.[1] Hence, a high degree of suspicion is necessary for suspecting it. Any recalcitrant lesion of the nail unit with nail plate destruction must raise suspicion and must be biopsied. Histopathological diagnosis is confirmatory from an adequate biopsy.[2]
This report discusses the clinical presentation, diagnosis and treatment of SCC in an elderly female, highlighting the importance of vigilance in the evaluation of a recalcitrant, long-standing nail unit lesion.
CASE REPORT
A 53-year-old female presented to our dermatology outpatient department with a solitary, painless growth on her right index finger, present for the past 4 years. It used to bleed on manipulation. The patient reported no history of trauma or other predisposing factors. She had been taking various treatments from private practitioners without any response. Clinical examination revealed a well-defined, 1*1 cm sized erythematous, hypertrophic plaque with overlying haemorrhagic crusts, involving the periungual aspect of the right index finger [Figure 1]. There was no regional lymphadenopathy. Dermoscopic examination showed superficial white scales, white structureless areas, blood clots, and linear and irregular vessels [Figure 2]. Based on the history, clinical and dermoscopic examination, pyogenic granuloma, irritated verruca vulgaris and SCC of the nail unit were kept as differential diagnoses.

- A well-defined, erythematous and hypertrophic plaque with overlying haemorrhagic crusts, present on the periungual aspect of the right index finger.
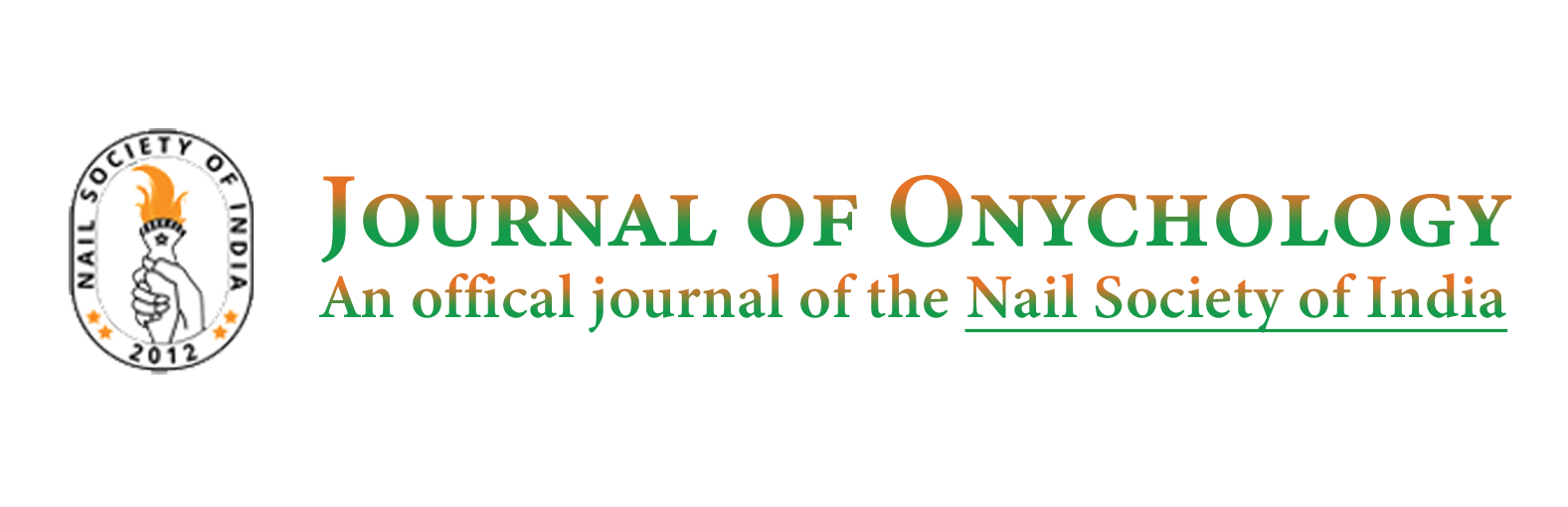
- Onychoscopy showing superficial white scales, white structureless areas (blue star), blood clots (green arrow), and linear and irregular vessels (orange arrow).
On investigation, X-Ray of the finger did not reveal any bony involvement. Doppler ultrasound revealed distal palmar branches showing biphasic blood flow without any evidence of intraluminal thrombus. Contrast-enhanced magnetic resonance imaging (MRI) scan revealed an altered intensity in the perionychium of the lateral aspect of the right index finger. The enhancement was suggestive of paronychia of the right index finger. No perineural or lymphovascular invasion was noted on MRI.
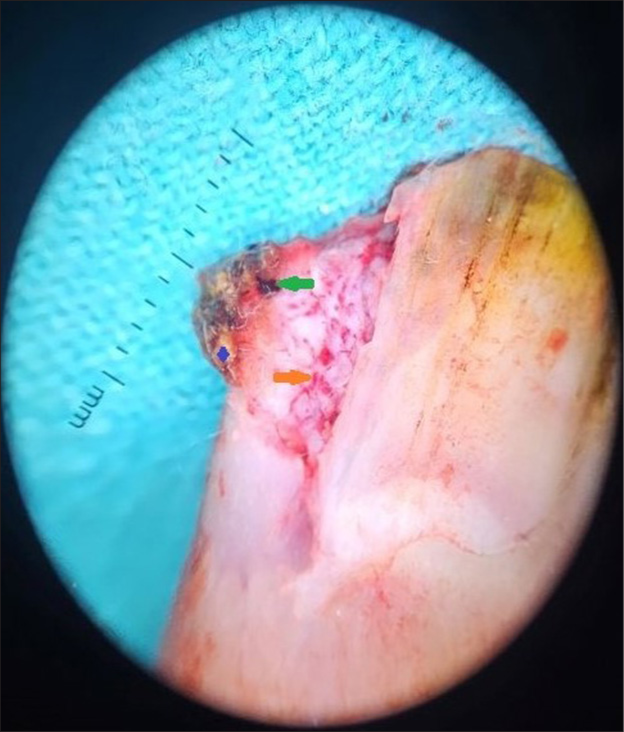
An excisional biopsy was performed [Figure 3a and b], and histopathological examination revealed a tumour consisting of nests of atypical squamous cells with abundant eosinophilic cytoplasm, with vesicular and hyperchromatic nuclei. It was extending into the entire epidermis and dermis, with central keratinisation and pearl formation, consistent with well-differentiated SCC [Figure 4].
- (a) Appearance of finger post-procedure. (b) Side view of finger post-procedure.
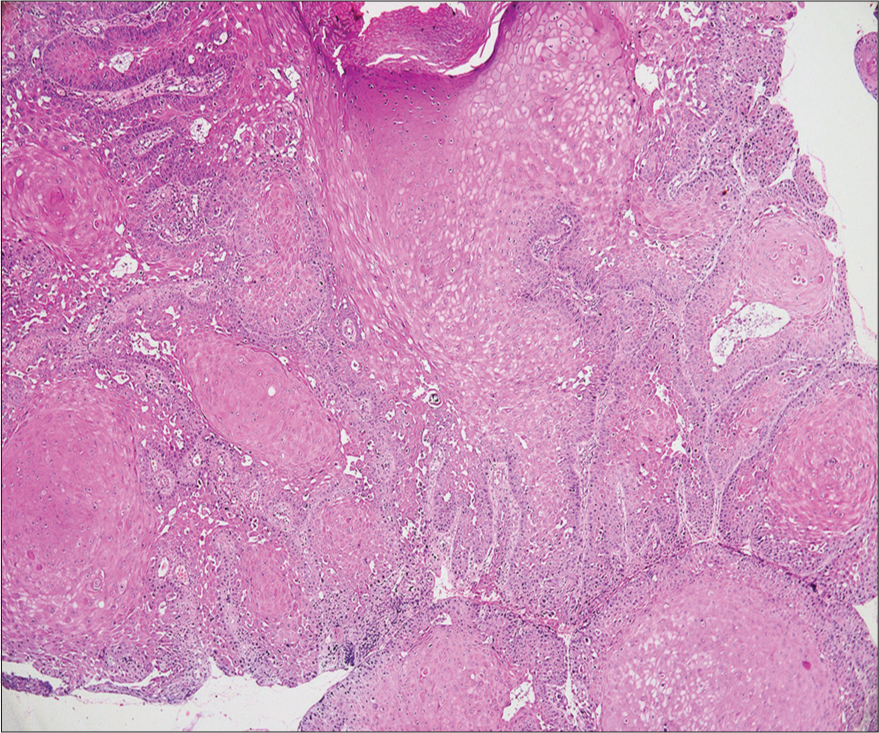
- Nests of atypical squamous cells with abundant eosinophilic cytoplasm, with vesicular and hyperchromatic nuclei, extending into the entire epidermis and dermis (Hematoxylin and eosin ×40).
Based on histopathological findings, the patient was referred to a surgical oncologist for further management. Wide local excision was performed by the surgical oncologist in order to achieve negative margins. Histopathological examination was performed which revealed no remnants of the disease. The patient was advised regular follow-up.
DISCUSSION
Squamous cell carcinoma of the nail unit is an uncommon neoplasm. It has a peak incidence in the 5th and 6th decades. Due to its rarity and lack of awareness, the diagnosis is often delayed.[1] The suggested aetiological or predisposing factors include trauma, chronic infections, human papillomavirus infection, burn scars, radiation exposure, chronic radiodermatitis and chronic exposure to sun.[3] Nail unit SCC has an indolent course with a low risk of metastases. It presents with non-specific features such as pain, nail plate destruction or discolouration, erythronychia, subungual hyperkeratosis, onycholysis, ulceration, periungual or subungual mass with intermittent bleeding or paronychia and nodule formation.[4,5] Bone involvement is seen in more than 20% of cases, ranging from 16% to 66%, being more common in immunocompromised patients.[5,6] The tumour may simulate other conditions such as pyogenic granuloma, verruca vulgaris, onychomycosis, onychopapilloma, longitudinal melanonychia, subungual exostosis, chronic paronychia, fibrokeratoma, onychomatricoma, amelanotic melanoma, verrucous carcinoma and subungual keratoacanthoma.[5,7]
An accurate diagnosis of nail unit SCC is based on a combination of clinical examination, onychoscopy, imaging and histopathological analysis. Typical onychoscopic features of nail unit SCC include characteristic vascular features, pigmented structures and other dermoscopic features.[8,9] Vascular features include dotted vessels, irregular vessels, curved vessels, sagittal vessels, ‘milky-red areas’, linear and regular vessels, coiled and hairpin vessels and arborising vessels. Pigmented structures described include dotted purpura, grey granulation and splinter haemorrhage. Other onychoscopic signs include pink background, translucent structureless areas, whitish scaly areas, distal plug, yellowish scales and dots and ‘digitiform’ proximal edge.[8,9]
On ultrasonography, nail unit SCC appears as a heterogeneously hypoechoic focal mass with irregular margins. Doppler mode shows low-resistance pulsatile flow signals within the tumour or at the periphery.[6] A radiological examination is needed to identify underlying bone involvement, which, if present, necessitates amputation. It should be kept in mind that X-ray of the digit may show osteolysis due to compression and not due to true bone invasion.[5,6] In case of true bony invasion, X-ray and computed tomography are useful in depicting a crescent-shaped, soft-tissue mass with osteolytic defect of the underlying phalanx without periosteal reaction. MRI is performed to identify the exact location and extension of lesions and, thus, aids in local staging for SCC.[5]
The diagnosis can be confirmed by performing an appropriate biopsy followed by histopathologic evaluation. A variable degree of irregular and incomplete keratinisation may be seen with superficial ulceration. A high degree of atypia with large and hyperchromatic nuclei in the basal and spinous cells, single-cell necrosis, and pathological mitoses are observed with frequent keratin pearls. The epidermis shows vacuolated superficial keratinocytes with pyknotic raisin-like nuclei.[2]
The treatment of nail unit SCC aims to achieve complete tumour removal while preserving the function and cosmetic appearance. Treatment modalities include wide local excision, Mohs micrographic surgery, digital amputation and radiotherapy. Mohs micrographic surgery provides the highest cure rate for the treatment of nail SCC and should be considered as the first-line approach.[6,8] The prognosis depends on several factors including tumour size, depth of invasion, and histological grade. Regular follow-up is essential to monitor for recurrence, given the risks associated with SCC.
This case emphasises the importance of considering SCC in the differential diagnosis of any chronic, recalcitrant, non-healing lesions, irrespective of its location. Although the patient remained undiagnosed for a few years, surgical management resulted in removal of the lesion entirely leaving no remnants. The patient was then kept under follow up. Complete removal of the lesion, leaving behind no remnants, helped ensure a favourable outcomein our patient.
CONCLUSION
Our case had an unusual presentation mimicking a pyogenic granuloma and hence was being misdiagnosed for a long time. Only the histopathological evaluation revealed it is SCC. Any chronic nail lesion, especially with verrucous morphology, with atypical characteristics should always be biopsied.
Authors’ contributions
IM: Performing the procedure, Preparing the manuscript; SB: Supervising the procedure, Proof reading the manuscript; SS: Providing the histopathological images, Providing the histopathological diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Shikha Bansal is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Squamous cell carcinoma of the nail bed. Chin Med J (Engl). 2017;130:877-8.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma of the nail unit: A clinical histopathologic study and a proposal for classification. Dermatol Surg. 2019;45:365-70.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma of the nail bed: Three case reports. J Orthop Surg (Hong Kong). 2004;12:248-52.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol. 2013;69:253-61.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma of the nail unit: Review of the literature. J Hand Surg Am. 2018;43:374-9.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma of the nail unit. Dermatol Pract Concept. 2018;8:238-44.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma of the thumb nail bed. Indian J Dermatol Venereol Leprol. 2007;73:445.
- [CrossRef] [Google Scholar]
- Intraoperative dermoscopy features of subungual squamous cell carcinoma: A study of 53 cases. Clin Exp Dermatol. 2021;46:82-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of melanoma and non-melanoma skin cancers. Front Med (Lausanne). 2019;6:180.
- [CrossRef] [PubMed] [Google Scholar]